Redesigned pulse oximeter advances more equitable healthcare
Redesigned pulse oximeter advances more equitable healthcare
The team’s innovative design gives healthcare providers a more accurate way to diagnose and treat hypoxemia — low levels of oxygen in the blood — in patients of color by correcting for the presence of melanin in skin before estimating blood oxygen levels. Hypoxemia causes symptoms like headaches, difficulty in breathing and rapid heart rate.
“This not only improves the quality of life for patients, but also reflects the need for devices that mitigate potentially overlooked inequity in healthcare,” explains Wubin Bai, assistant professor of applied physical sciences.
Current options for pulse oximeters measure how much oxygen is in an individual’s blood by analyzing light absorption through the finger to estimate blood oxygen levels. In 2021, the Food & Drug Administration (FDA) issued an alert on limitations of pulse oximeters stating that inaccurate or inconsistent readings may result from factors including poor circulation, dark skin pigmentation, thick skin, tobacco use, and more. The FDA advised that numbers from pulse oximeters should not be used in isolation to determine an individual’s health as existing technology mostly relies on absorption numbers that do not consider skin tone.
Specifically, as the primary pigment present in many people of color, melanin affects the accuracy of oxygen measurements. Thus, many pulse oximeters may overestimate blood oxygen levels, especially for people of color, potentially causing inaccurate diagnoses and delayed treatment.
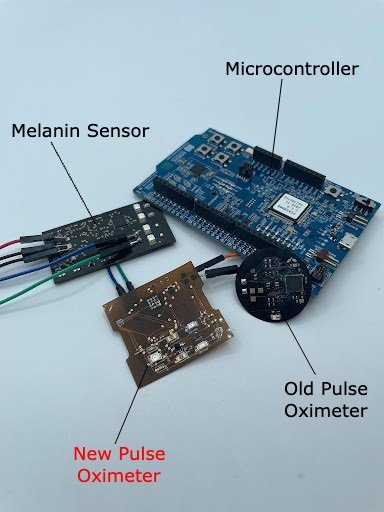
To remedy this issue, the Bai lab collaborated with a team of researchers to develop a more practical and cost-effective solution that works as an “add-on” to existing processes. Bai explains his group’s pulse oximeter is a wearable, flexible patch that is placed on the skin for measurement and features a low-cost construction to enable additional sensing to counteract confounding effects, such as skin melanin.

According to the team, the final product may promote important discussions about how biases in healthcare can affect clinical decisions and illuminate inequities in treatment.
“The previously held assumption that melanin does not impact readings significantly was never tested properly until it was already fully implemented into our current healthcare infrastructure,” Putcha says. “This is reflective of inherent biases in healthcare which further perpetuate inequities within the existing system.”
“These combined non-invasive and wearable sensing capabilities provide promising routes to precision medicine for inclusion and equity,” adds Bai. The technology will hopefully be produced and implemented en masse in healthcare facilities across the globe to ultimately “mitigate health disparity and enhance sensing accuracy and stability.”
Currently, a provisional patent has been filed and accepted through the UNC Office of Technology Commercialization and the team plans on filing for the full U.S. patent by next August. Clinical trials are expected to commence in the near future.